1. A JC is an academic session where we go through a scientific article for 1 hour.
2. It takes place every Friday.
3. Its purpose is to understand and discuss relevant elements about the content taking interactive and pedagogic notes (highlighting, underlining and using other learning resources) about the content.
4. We generate further appraisal, identify the opportunities of learning and formulate some potential research questions.
5. We write down the key-points of every session and publish them on our website
6. The article for the next session is posted one week in advance the must-read JC channel of our DISCORD server.
2018 CID - Renal Dosing of Antibiotics Are We Jumping the Gun (Crass) [r].pdf
Codified by ABFL
Glossary:
🪲 = microorganisms;
♾ = renal;
ATB = antibiotics;
Ccr = creatinine clearance;
CKD = chronic kidney disease;
1. EVIDENCE
- ATB dose adjustments applies for stable CKD
- May not apply to late late-phase trials and practice.
- Ceftolozane/tazobactam, ceftazidime/avibactam, and telavancin ➩ all have precautionary
statements for ↓ clinical response (Ccr 30-50) ➩ no need to adjust doses
2. ATB elimination is mostly relevant in acute cases during the 1st 48h
3. Toxicity + efficacy should be considered in every ATB
4. FDA ➩ inferior EFFICACY in moderate ♾ impairment.
5. GOAL ➩ Keep efficacy with the ↓ toxicity possible.
6. CKD studies available in CKD are small, early phase of healthy
7. “Antibiotics do not fit cleanly into this paradigm due to overwhelmingly episodic, rather than
chronic, use.” Crass 2018
⏳ TIME MANAGEMENT.
01:22:41
Round: 5 01:11:57 Comments
Round: 4 27:19:13 JC main points
Round: 3 32:18:27 JC intro
Round: 2 12:30:77 Codification discussion
Round: 1 09:21:62 Past JC
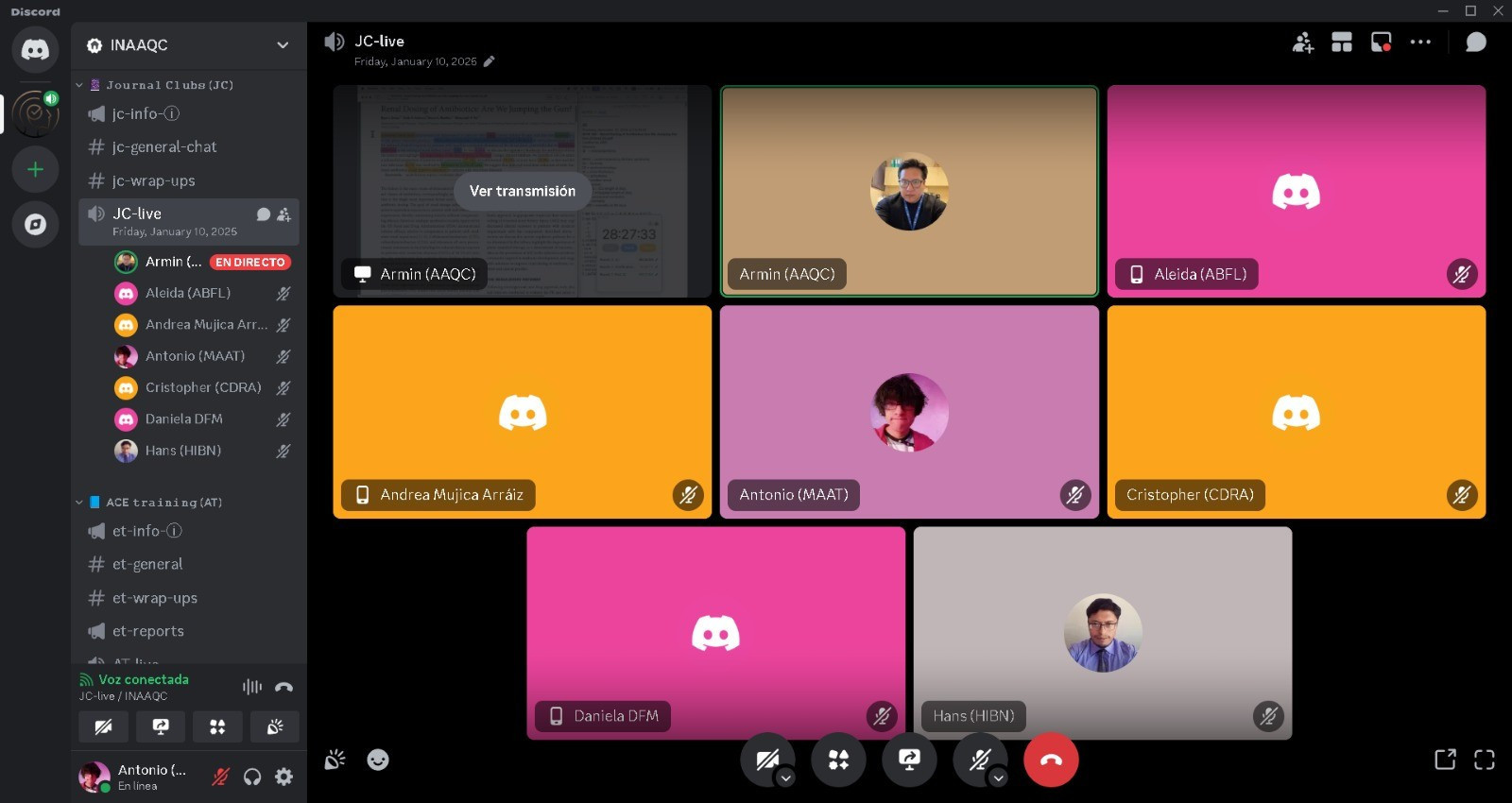
Friday, January 10 , 2025 at 18h30 at BO - 23h30 at BE
ABFL, CORA, AMA, MAAT, DFM, HIBN, AAQC
Codified by MAAT
Glossary: 🫁 = lungs; 🤔 = analysis; ⏎ = return; ARDS = acute respiratory distress syndrome; BLUE = The American Journal of Respiratory and Critical Care Medicine.
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2024, BLUE, FR ➖ retro_prag_🤔 - cohort ➕ 41pxs ➕ 8y (2014 - 2022) ➖ P I C O:
- P: adults + ECCO2R
- I: Vt ≤3mL/Kg (ultra-protective vent)
- C: NA
- O: p_OC = feasibiliy (proportion of sessions) ➖ s_OC = efficacy + safety + others (adverse
events, SS90)
3. EVIDENCE: - …
⏳ TIME MANAGEMENT.
01:13:20
Round: 4 10:34:78 Comments
Round: 3 51:30:02 ART ultra-low volume ventilation
Round: 2 05:36:00 Select ART
Round: 1 05:39:31 Past JC
Friday, January 3 , 2025 at 18h30 at BO - 23h30 at BE
ABFL, CORA, AMA, MAAT, DFM, HIBN, AAQC
Friday, January 24 , 2025 at 18h30 at BO - 23h30 at BE
ABFL, MAAT, JCAU, HIBN, MACR, GMC, AMA, AAQC
2021 HHP - How many fruits+vegetables do we really need (Circulation).pdf
2021 CIRCULATION - Fruit and Vegetable Intake and Mortality, 2 Prospective Cohort Studies + MA of 26 Studies (wang) [MA]
Codified by ABFL
Codified by ACE ᵗᵉᵃᵐ
Glossary:
🫁 = lungs, COPD; 🧠 = brain, stroke; 🫀 = heart, cardiovascular disease; WHO = World Health Organization; WCRF = World Cancer Research Fund; NHSE = National Health Service of England
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2021, CIRCULATION, USA ➖ obs_PROS + MA ➕ 2M | pros = >66k in ♀ (1984-2014) – >42k iin ♂ (1986-2014) ▶ MA = 1.8M ➕ 30y ➖ P I C O:
- P: adults
- I: pooled self-reported health and diet information
- C: NA
- O: MM ➩ Results:
• 10%. ↓r CA - (0.90)
• 12%. ↓r 🧠 🫀 (HR 0.88)
• 13%. ↓r MM (HR 0.87)
• 15 35%. ↓r 🫁 COPD (0.65)
3. EVIDENCE:
- Leafy green vegetables: kale + spinach
- Fruits & vegetables: vitamin C + beta carotene (ANTIOXIDANTS)
- NO BENEFIT in MM ➩ >5 servings OR starchy veggies OR potatoes OR drinking fruit juices.
- Veggies only = no ↓ CA (p=0.62)
- RECCO diver among countries ➩
* 8.5 servings in AUS
* 6 servings in DEN
* 5 servings in WHO, WCRF, NHSE
- Fruit juices + potatoes = ↑ glycemic load (various DIETARY RECOMM include them)
- How much you eat in average MATTERS ➩ if NOT achieved THE GOAL, you can
compensate the day after.
⏳ TIME MANAGEMENT.
01:27:38
Round: 8 00:01:30 The end
Round: 7 06:31:64 Wrap-up
Round: 6 12:09:86 Images + keypoints
Round: 5 37:44:75 ART 1 original
Round: 4 21:01:46 ART 1 prequel
Round: 3 04:19:04 Selection
Round: 2 02:13:15 Past JCRound: 1 03:37:75 Past JC
Codified by MAAT
Glossary:
♾ = kidneys; ABW = actual body weight; AKD = acute kidney disease;
CH = Switzerland; coh = cohort; DE = Germany; h_DIS = Hospital discharge; IBW = ideal body weight;
mc = multicentric; UO = urinary output.
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2024, CC, CH + USA ➖ mc_coh ➕ 15,322 + 28,610 (derivation + validation) ➕ CH 2010-2020 ➖ P I C O:
- P: adults, CI pxs
- I: CH (Laus’AKI, derivation coh) 🆚 USA (MIMIC-IV, validation coh)
- C: NA
- O: best predictor for UO
3. EVIDENCE:
- Oliguria = <0.5mL/Kg/h in ≥6h
- Presents in 75% of CI pxs + ↔ MM90
- Estimation of weight is inaccurate
- ABW ➩ massive variations (fluid overload + muscle mass loss + obesity + underweight)
- Types of BW: pre-admission + actual + ideal + adjusted
- Series (493 pxs = overestimation) + 2 large studies (USA + DE = confirmed)
- 4th study (S + 569pxs) not influenced by the method (oliguria & MM)
- The four studies = single center
4. METHODS.
- DEF ➠ Best predictor for UO = most closely ↔ w_mean UO d_UCI
- IN ➠
* Laus’AKI: ≥18yo, Lausanne, Jan 2010 - Jun 2020
* MIMIC-IV: Boston, 2008 - 2019
- EX ➠
* Laus’AKI + MIMIC-IV: refused, u_HD, <6h UO measurement, no sCr, no weight, no height,
vesical irrigation d_ICU stay.
- RANDOM ➠
- INTERV ➠ 1st. Best predictor was chosen 2nd. Compared OLIGURIA INCIDENCE w_: a. MM90, b. AKD at H+dis ➩ according to ABW or IBW (which normalized better)
6. RESULTS
- USA cohort: heavier, older, lower in SAPS-II (than CH cohort)
- Best UO predictor = IBW (‘oliguria incidence’ was constant)
- IBW ➩ ↗️ association ↔ oliguria w_: MM90 & AKD
- After correction (sex, SAPS-II): ALL FINDINGS PERSISTED
Friday, January 17 , 2025 at 18h30 at BO - 23h30 at BE
ABFL, MAAT, JCAU, HIBN, MACR, GMC, AMA, AAQC
⏳ TIME MANAGEMENT.
01:18:15
Round: 5 06:07:41 Figures
Round: 4 20:28:69 Content + wu
Round: 3 33:11:79 Article UO
Round: 2 06:06:67 Article choice
Round: 1 12:21:18 Past JC
Codified by MAAT
Glossary:
💨 = flow = perfusion; 🫁 = lungs; 🫀 = heart; FC = fluid challenge; FR = fluid responsiveness; PPV = pulse pressure variation.
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2025, CC, UAE ➖ srMA ➕ 5 studies (474 pxs) ➕ PROSPERO - publication (1y) ➖ P I C O:
- P: ↓Vt
- I: ∆PPV & ∆PPV% a_PLR following ‘…not a drop of fluid’
- C: fluid challenge or response to PLR
- O: ability to predict FR in ↓ Vt MV
3. EVIDENCE:
- 1st line therapy = fluid administration ➩ tissue hypoperfusion context
- FC AIM = ↑ preload + CI ➩ 🔝 DO2 + tissue 💨
- Excessive fluid ➩ peripheral + 🫁 edema + poor OC
- Deficient fluid ➩ MOF + MM
- 50% are fluid responsive- PPV accurately predicts FR in MV pxs ➩ only if Vt ≥8 ➩
OTHERWISE (Vt <8), insufficient to induce changes in THORACIC PRESSURE &
PRELOAD.
Friday, January 31 , 2025 at 18h30 at BO - 23h30 at BE
AMA, HIBN, AAQC
⏳ TIME MANAGEMENT.
01:28:32
Round: 4 06:18:93 Comments
Round: 3 01:07:40 ART
Round: 2 09:17:00 ART selection
Round: 1 05:16:43 Past JC
2025 CC - Cardiovascular effects of lactate in healthy adults (berg-hansen) [R].pdf
Codified by MAAT
Glossary:
🫀 = heart; AHF = acute heart failure; CABG = coronary artery bypass graft; eo_PER = end organ perfusion; GFR = glomerular filtration rate; GLS = global longitudinal strain; Ea = effective arterial elastance; HEC = hyperinsulinemic-euglycemic clamp; LAC = half-molar lactate; Lac 45g/L + Na 15g/L; MAP = mean arterial pressure; SAL = sodium-matched hypertonic sodium chloride; Na 15g/L, Cl 23 g/L; SV = stroke volume; SVR = systemic vascular resistance. .
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2025, CC, DK ➖ RCT, single-blinded, crossover ➕ 8 ➕ March - June 2021 ➖ P I C O:
- P: healthy
- I: LAC (4h infusion)
- C: SAL
- O: CO (by ECHO); sOC = SV, LVEF, GLS, Ea, SVR
3. EVIDENCE:
- Usually large amounts of fluids are needed to ↑ CO + ↗ eo_PER
- No consensus about the optimal type of fluid resuscitation.
- MORTALITY = ↑ fluids OR ↓ fluids
- Small-volume resuscitation w_hypertonic saline ➩ proposal ➩
* ➕ : ↗ CO + vascular tone + microcirculation.
* ➖ : Careful w_hyperchloremia + metabolic acidosis
* ➖ : ♾ vasoconstriction + ↓ GFR
- Hypertonic crystalloid solutions
* ➕ : ↗ HD effects wo_chloride + ↗ eo_PER & CO (AHF + af_CABG)
4. METHODS.
- IN ➠ ♂ + ≥18yo + BMI 18-30
- EX ➠ daily med + abnormalities in routine screening tests + acute or chronic disease
(known 🫀 failure)
- RANDOM ➠ 14 day interval (minimum) = washout
* ⊖ strenuous physical activity + alcohol
* ⊕ regular diet for 48h before each study day
- INTERV ➠ ECHO + blood samples
* T0, 60, 120, 240
* HEC was used at 180 min (main study) ➩ 240min was w_HEC
* HEC = insulin (0.6mU/Kg/min) + glucose (20%)
- CONSORT was used (as stated by Equator)
6. RESULTS. LAC 🆚 SAL
- LAC ↑ :
1. Lactate = ↑ 1.9mmol/L
2. CO = ↑ 1L/min = due to SV of 11mL
3. LVEF = ↑ 5 percentage points
4. GLS = ↑ 1.5 percentage points
5. Contractility = ↗
- LAC = :
1. HR = no change
2. MAP = similar
- LAC ↓ :
1. Afterload (SVR + Ea)= ↓
- SAL:
1. Preload indicator = ↑
7. RATIONALE
- ↗ 🫀 function ➩ ↑ CO, SV, LVEF in LAC
- Contractility ↗ ➕ afterload ↓ ➕ preload = (stable)
⏳ TIME MANAGEMENT.
01:29:52
Round: 8 03:32:41 Comments
Round: 7 27:45:06 Wrap-up
Round: 6 15:06:89 Figures
Round: 5 17:55:76 Methods
Round: 4 06:36:59 Intro
Round: 3 11:21:90 Abstract
Round: 2 01:17:91 ART selection
Round: 1 06:16:33 Past JC
Friday, February 14, 2025 at 18h30 at BO - 23h30 at BE
AMA, MACR, DFM, JQB, MAAT, HIBN, AAQC
CC 2015 - Passive leg raising, five rules, not a drop of fluid (monnet, teboul).pdf
1. ↑ 300mL venous blood from ↓body → right 🫀
2. 5 rules:
- 1st. Start from semi-recumbent position ▶ 1 study = poor reliability if this rule is not
followed
- 2nd. Measure CO ▶ not w_BP only (mechs: arterial compliance + pulse wave
amplication) ▶ HOWEVER, MAP ≥10% could be a good predictor. (2016 CHEST -
Passive Leg Raise Prediction of Fluid Responsiveness Using Nicom and Flatcar Devices
in Septic Shock: Preliminary Findings. It worked w_NICOM)
- 3rd. In 1 min. ▶ Real time CO measurement is needed
- 4rd. Measure CO a_PLR
- 5th. Do not touch (avoid adrenergic stimulation) ➕ PLR does not ↑ HR
Codified by MAAT
Glossary:
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2025, CC, UAE ➖ srMA ➕ 5 studies (474 pxs) ➕ PROSPERO - publication (1y), till Aug 2024 ➖ P I C O:
- P: ↓Vt
- I: ∆PPV & ∆PPV% a_PLR following ‘…not a drop of fluid’
- C: fluid challenge or response to PLR
- O: ability to predict FR in ↓ Vt MV
3. EVIDENCE:
- 1st line therapy = fluid administration ➩ tissue hypoperfusion context
- FC AIM = ↑ preload + CI ➩ 🔝 DO2 + tissue 💨
- Excessive fluid ➩ peripheral + 🫁 edema + poor OC
- Deficient fluid ➩ MOD + MM
- 50% are fluid responsive
- PPV accurately predicts FR in MV pxs ➩ only if Vt ≥8 ➩ OTHERWISE (Vt <8 of ideal body
weight), insufficient to induce changes in THORACIC PRESSURE & PRELOAD.
- PLR is an ACCUTE METHOD to predict FR in ↓ Vt (real-time CI is needed)
- Real-time CI NOT ALWAYS AVAILABLE ➩ or technically ineligible (ECHO echogenicity)
- PPV after PLR = good method (predict FR) ➩ SBA + ↓ Vt + MV pxs + PO critILL pxs (2021 - 2024) ▶ ROC curve issues (0.78 to 0.98) + wide 95%CI
4. METHODS.
- IN ➠ PubMed, Embase, Cochrane
- INTERV ➠
- ∆PPV = end_PPV - baseline_PPV
- ∆PPV% = end _ PPV - baseline_PPV) / baseline_PPV 1 x 100 ▶ baseline = the patient in
the 45 semi-recumbent position BEFORE PLR test
- A PLR test was then performed using an automatic elevation bed by raising the patient’s
lower limbs to a 45 angle while the patient’s trunk was lowered from a semi-recumbent to
supine position with no changes in the hip angle
- …
💨 = flow = perfusion; 🫁 = lungs; 🫀 = heart; CI = cardiac index; FC = fluid challenge; FR = fluid responsiveness; MOD = Multiorgan disfunction; PO = postoperative; PPV = pulse pressure variation; SBA = spontaneous breathing activity.
⏳ TIME MANAGEMENT.
01:38:37
Round: 4 12:19:53 Wrap-up
Round: 3 42:23:90 PLR technique
Round: 2 37:11:54 JC
Round: 1 06:42:31 Past JC
Friday, February 7 , 2025 at 18h30 at BO - 23h30 at BE
DFM, AMA, DD, HIBN, AAQC
2024 JACC - From ST-Segment Elevation MI to Occlusion MI (McLaren) [r].pdf
Codified by AMA
Glossary:
ACC = American College of Cardiology, ACO = acute coronary occlusion, INT = interpretation, MI = myocardial infarction, OMI = occlusion MI, STEMI = ST-segment elevation MI.
1. Q-wave/non-Q wave ➩ STEMI 🆚 non-STEMI ➩ OMI
2. 25% from non-STEMI have ACO ➩ limitation
3. OMI rises based on ✔ or ✖ of ACO
4. OMI paradigm = advanced ECG (INT aided by AI ➕ ECHO ➕ imaging ➕ refractory
ischemia (clinical signs).
5. Benefits of OMI paradigm = opportunity to transform ER 🫀 +↗️pxs care.
6. Thomas Kuhn introduced the concept of PARADIGM SHIFT
7. To guide problem solving activities ➩ definition + methods
8. 2021 CIRCULATION ➩ although the dichotomuos classification (STEMI/non-STEMI), IT IS
LIKELY that the main pathophysiological event is ACUTE VESSEL OCCLUSION
(determining prognosis + natural history).
9. ACC consensus (2022) ➩ STEMI criteria (12-lead ECG) misses A SIGNIFICANT MINORITY
of pxs w_ACO.
10. Alencar, 3 studies ➩ STEMI criteria for ACO = sensibility 44%
⏳ TIME MANAGEMENT.
01:09:58
Round: 5 01:33:50 Comments
Round: 4 13:41:71 wrap-up
Round: 3 34:16:12 ART
Round: 2 08:23:64 ART selection
Round: 1 12:03:40 Past JC
Friday, February 28 , 2025 at 18h30 at BO - 23h30 at BE
AMA, MAAT, GMC, MACR, HIBN, AAQC
Codified by AMA
Glossary:
C19 = COVID-19; DIS = discharge; HRQoL = health-related quality of life; ICU-VR = intensive care unit virtual reality; MH = mental health; PICS-F = post-intensive care syndrome-family; PTS = post-traumatisc stress; rel = relatives; SOC = standard of care; TECH = technology
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2025, CC, NL ➖ mc_px-cluste_RCT ➕ 189 rel ➕ 1y3m = Jan 2021 - Apr 2022 (+6m after DIS) ➖ P I C O:
- P: rel (adult pxs)
- I: SOC + ICU-VR (100 rel of 81 pxs)
- C: SOC (89 rel of 80 pxs)
- O: symptoms of MH distress (DIFF ↔ prevalence + severity of PTSD + anxiety +
depression). sOC = understanding of ICU environment & procedure ➕ perspectives
toward ICU-VR
3. EVIDENCE:
- Mental health challenges in CI pxs’ rel: PTS + anxiety + depression
- MH sequealae
4. METHODS.
- IN ➠ rel 1st or 2nd degree ➕ ICU stay ≥72h ➕ multiple rel could participate
- EX ➠ language barrier ➕ no TECH ➕ no formal 🏡 address.
- RANDOM ➠ all relatives from one px were assigned to the SAME GROUP (↓ r of cross-
contamination) ➩ STRATIFIED in centers ➕ ability to visit the hospital (C19)
- INTERV ➠ 48h after admission (time to approach the rel) ➕ rel could share the study-
relation info
* 14 min
* Voice-over pre-recorded
* Mock patient lying
6. RESULTS
- Baseline, discharge, 1, 3, 6 months ➩ study periods (questionnaire)
- NO DIFF in pOC
- DIFF on understanding of ICU treatment ➕ perception/perspective on ICU-VR ➩ BOTH ↗
7. RATIONALE
* A more tailored, multifaceted approach, incorporating a combination of interventions like ICU-VR at different stages of the ICU experience may prove more effective.
8. LIMITATIONS
- Not blinded to rel & investigators (blinded to researcher)
⏳ TIME MANAGEMENT.
01:25:47
Round: 7 07:25:35 Comments
Round: 6 11:46:41 Results
Round: 5 30:00:94 Methods
Round: 4 16:27:26 INTRO
Round: 3 11:42:31 JC, abstract
Round: 2 03:16:61 ART selection
Round: 1 05:08:43 past JC
Friday, February 21 , 2025 at 18h30 at BO - 23h30 at BE
AMA, MAAT, DFM, MACR, HIBN, AAQC
Friday, March 14 , 2025 at 18h30 at BO - 23h30 at BE
AMA, MACR, DFM, JQB, MAAT, HIBN, AAQC
2024 JACC - From ST-Segment Elevation MI to Occlusion MI (McLaren) [r].pdf
Codified by ABFL
Glossary:
ACC = American College of Cardiology, ACO = acute coronary occlusion, Computerized Tomography, Delayed Invasive Intervention in Patients With Non–ST-Segment–Elevation Myocardial Infarction, INT = interpretation, MI = myocardial infarction, OMI = occlusion MI, RIDDLE-NSTEMI = Randomized Study of Immediate Versus, STD = ST-segment depression, STEMI = ST-segment elevation MI, TIMACS = Timing of Intervention in Acute Coronary Syndromes, VERDICT = Very EaRly vs Deferred Invasive evaluation using.
1. Image of non-STEMI = STEMI (occluded) + non-STEMI (nonocclusive thrombus)
2. Clear deviation from actual evidence ➩ real occlusion in non-STEMI
3. ST criteria (age, sex) = Healthy 🆚 CKMB measured MI pxs ➩ DESPITE THIS… REC
differentiation of MI w_ & wo_ACO
4. NORMAL SCIENCE = persistence of a paradigm (successful in its aim, steady expansion) =
DOES NOT aim at novelties
5. OCs of STEMI criteria ➩ best reperfuse + ↓ reperfusion delays
6. STEMI paradigm ➩
* ↗️REPERFUSION strategies & techniques
- Angiography
- Stenting
- Medications
- Door-to-balloon (time is myocardium)
* ↗️🫀 ER + INTERdisciplinary collaboration:
- ⊕ Cath lab
- Paramedics BYPASSING ER departments
- Rapid assembling of interventional 🫀 teams
* 2 quality ↗️:
- ↓ reperfusion delays
- ↓ false positives STEMI
* NOVELTY:
- No false negatives found ➩ ECG wo_STEMI criteria + ACO = NOT considered a false
(-) STEMI ➩ “As a result, the patient will be denied emergent reperfusion”
- McLaren stated this problem in 2023 AJEM, Missing occlusion
* Evidence
- Trials have not regarded this type of cases
- Many non-STEMI trials have reperfusion time limitations ➩ TIMACS 16h (unstable
angina, non-STEMI) to reperfusion.
- VERDICT (unstable angina, non-STEMI) = benefit from 4.7h of reperfusion.
- RIDDLE-NSTEMI = ↓ MM in immediate reperfusion
- NSTEMI exclude refractory ischemia OR HD/electrical instability
- 6.4% of VERY-HIGH NSTEMI ➩ angio in 2h
⏳ TIME MANAGEMENT.
01:24:22
Round: 4 00:50:82 Comments
Round: 3 23:33:13 wrap-up
Round: 2 47:53:53 JC
Round: 1 12:05:49 Past 2 JCs
⏳ TIME MANAGEMENT.
01:25:47
Round: 7 07:25:35 Comments
Round: 6 11:46:41 Results
Round: 5 30:00:94 Methods
Round: 4 16:27:26 INTRO
Round: 3 11:42:31 JC, abstract
Round: 2 03:16:61 ART selection
Round: 1 05:08:43 past JC
2024 JACC - From ST-Segment Elevation MI to Occlusion MI (McLaren) [r].pdf
Codified by ABFL
Glossary:
ACC = American College of Cardiology, ACO = acute coronary occlusion, INT = interpretation, MI = myocardial infarction, OMI = occlusion MI, STEMI = ST-segment elevation MI.
1. SHIFT ➩ scope + precision change OR stay when PARADIGM is more successful (few
problems resolved) - acute ones
2. STEMI criteria as SURROGATE of ACO = limited in scope + precision
3. 1994 MA ➩ “ECG w_STEMI criteria = emergent reperfusion”
- Suspected MI
- w_limited or NO ECG
- Treated w_streptokinase
- MI determined by CK-MB
- CRUDE separation = poor definition
- 4 studies ➩ no ECG requirements for enrollment
- cautioned about denying reperfusion in patients without STE.
- Few deaths + data-dependent emphasis could be misleading
4. Kuhn ➩ paradigms start FLEXIBLE… and then become RIGID
5. GLs:
1. 1996 ➩ advised THROMBOLYTICS for hyper acute T or ST-seg depression V1-V4 from
POSTERIOR MI (experienced expertise is needed)
2. 1999 ➩ advised CLASSIFY “w_STE or LBBB” + “nonDx ECGs” (even being posterior
infarctions)
3. ∑ STEMI paradigm emerged w_2 ≠ entities: STEMI 🆚 non-STEMI
Friday, March 07 , 2025 at 18h30 at BO - 23h30 at BE
MAAT, HIBN, AAQC
2025 ICM - How we use ultrasound in the mm of weaning from MV (Tuinman) [ed].pdf
Codified by ABFL
Glossary:
🫁 = lungs, 🫀 = heart,🫃🏽 = abdomen = abdominal, AbP = abdominal pressure, af_ = after, antiISCHE = anti-ischemic, CCUS = critical care ultrasound, DE = diaphragm excursion, Di = diaphragm, DIS = disease, DYSF = dysfunction, DW = difficult weaning, HTA = hypertension, IAP = intraabdominal pressure, iFunction = impaired function, MIP = maximal inspiratory effort = maximal inspiratory pressure, MV = mechanical ventilation, PSIC = parasternal intercostal, PSLA = parasternal long axis, PSSA = parasternal short axis, SBT = spontaneous breathing trial, TECHS = techniques, TFdi = thickening fraction of the diaphragm, WF = weaning failure.
1. DW ➩ ↑ adverse clinical OCs➕ resources (limited healthcare)
2. DW = failure SBT ➩ causes of WF ▶ iFunction: 🫁 🫀 Di
3. CCUS ➩ valuable DX tool ➩ MV, weaning, readiness for weaning, causes of WF, 🫀–🫁 function, TTO response.
4. ABCDE-US ➩ pathophysioly of WF ➩ DX ➕ monitoring = CAUSE oF WF
1. ABCDE ➩
- it is an ADJUNCT to clinical parameter + physical examination
- Timing: MV > 48h
- Frequency: follow-up determined by a. Cause, b. Course DIS
2. 🫀:
- DYSF ➩ MOST frequent causes of WF
- 1st. TTE. views (PSLA, PSSA, apical 2, 3, 4, 5 chamber, subcostal) ➩ eye-balling: to
estimate SIZE + FUNCTION both ventricles ➕ wall abnormalities OR 🫀 effusion
- 2nd. TTE by educated in ECHO. If CAUSE not clear
- 3rd. TEE. Diastolic function (E/A and E/e’ ratios) when FAILING an SBT. Wall motion
abnormalities + 🫀 valves (stenosis + regurgitation)
- TTO ➩ fluid removal ➕ antiHTA ➕ antiISCHE
3. 🫁 :
- Aeration score + P.eff.
* QUALITATIVE ▶ 6 views DX cause of ARF (sliding, pleural abnormalities, lung
profiles ABC, pleural effusion, consolidation w_or wo_ air bronchograms) ➖
careful w_deterministic fashion interpretation
* QUANTITATIVE ▶ 12 views ➩ calculare 🫁 aeration score ➩ monitor 🫁
pathology over time
* r_extubation failure ▶ 8 views ➩ ← → SBT ➩
* ≥5 B-lines = extubation failure (independent fro LV filling presssures)
* OCs ▶ weaning readiness + WF cause + monitor DIS progression & TTO
response.
4. 🫃🏽:
- ↑ AbP ➩ can affect MECHS ∑ weaning
- US ▶ screen aspect FREE FLUID (↓ anechoic) 🆚 heterogenous (↑ echoic) +
septum (useful for the cause of free fluid)
- Paracentesis DX and TTO
5. Di:
- Highly prevalent ➩ DYSF of Di
- US: to exclude Di DYSF ➩ af_FAILED initial SBT
- DE = subcostal OR subxiphoid (liver OR spleen as acoustic windows)
* IF not clear ▶ use INTERCOSTAL (zone of apposition to DISPLACEMENT of
liver
OR spleen) = qualititve alternative.
* Measured d_spontaneous breathing wo_ventilator support.
* In cooperative PXS ➩ MIP to assess MAX excursion
- Contractility: TFdi (via INTERCOSTAL) ▶
* ↑ = edema ➖ fibrosis (careful)
* ↓ = atrophy
* DYSF = DE <20mm
* WF (predictive) = TFdi <30-35% ➕ DE <10-15mm
6. Extra-Di
- ExtraDi muscles help Di weakness ➩ successful SBT BUT potential WF
- Expiratory muscle atrophy = impairment of airway clearance ➩ WF
- US: PSIC + rectus abdominis muscle + external oblique, internal oblique &
transversus abdominis (same window).
- Consider always IAP (due to GEOMETRY + MOBILITY)
- Thickening fraction of INTERCOSTAL MUSCLES >10% = ↑r_WF
7. FUTURE DIRECTIONS
- CLINICAL trials ▶↗️ predictive performance of 🫁 + Di
- DX continuous data ▶ ↗️ predictive performance of 🫁 + 🆕 indications
- Advanced TECHS ▶ speckle tracking (quantification of perfusion + better function
estimation).
8. These measurements can be used to form a definition of diaphragm dysfunction, although
there is variation in this definition: It has been defined as a thickening fraction of less than
20% or a tidal excursion of less than 10 mm – 2019 UJ - A narrative review of diaphragm
ultrasound to predict weaning from MV, where are we and where are we heading (turton) [r]
Friday, March 28 , 2025 at 18h30 at BO - 23h30 at BE
AMA, AHO, GMC, HIBN, AAQC
⏳ TIME MANAGEMENT.
02:13:08
Round: 5 06:52:74 Comments
Round: 4 58:27:56 Wrap-up
Round: 3 46:41:93 ART
Round: 2 06:47:19 ART selection
Round: 1 14:19:46 past JC
Glossary (most used)
↑ = increase, ↓ = decrease,↗️ = improve,↘️ = worsen, 𝗘𝗫 = exclusion, 𝗜𝗡 = inclusion, ★ = recommendation(s), 🗣 = suggestion(s), critILL = critically ill, DX = diagnosis, h_LOS = Hospital length of stay, icu_LOS = ICU length of stay, inc_ = incident, MA = metaanalysis, mc = multicentric, MM = mortality, MM90 = mortality at 90 days, pxs = patients, pOC = primary outcome(s), sOC = secondary outcome(s), SS = survival, w_ = with, wo_ = without, RCT = randomized controlled trial, sr = systematic review, yo = years old.
Brief scope glossary
- 𝙄𝙌𝘾 BS 🟰 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ brief scope ↩
- Y, J, C ➖ T ➕ N ➕ t ➖ P I C O: ↩
- year (Y), journal (J), country (C) ➖ type of study (T) ➕ number of patients/sample (N) ➕ time (t) ➖ population (P),
intervention (I), comparison (C), outcome (O, OC).
Complete glossary here
Friday, April 11 , 2025 at 18h30 at BO - 23h30 at BE
HIBN, AAQC
2025 CC - Ventilation-induced AKI in ARF Do PEEP levels matter (Benites) [r].pdf
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
🫧 = alveolar, AF = atrial fibrillation, AKI = acute kidney injury, ARDS = acute respiratory distress syndrome, CA = cancer, GE = gastroenterology, MV = mechanical ventilation, Ppl = pleural pressure, VR = vascular resistance.
1. ARDS & MV
- ARDS = major issue in CIpxs
- MV = crucial for TTO, with PEEP (Positive End-Expiratory Pressure) being a key setting.
2. High vs. Low PEEP – The Debate
- ↑ PEEP:
* a.↗️🫁 compliance ➕ O2
* b. ❌ inconclusive effects ➩ MM or d_MV.
- ↓ PEEP:
* May ⊖ overdistension but r_↑ poor O2
- Optimal PEEP is still controversial.
3. Organ Crosstalk
- Improper PEEP affects: ❤️ 🧠 🧽
- ARDS pxs develop AKI (strong MM marker)
4. 🫁 - 🧽 crosstalk d_MV
- Gas Exchange Issues (↓O2, ↑CO2)
- Remote Biotrauma = Inflammatory mediators affecting distant organs
- HD changes = ↓ venous return + ↓ CO → Renal perfusion issues
5. h_PEEP & 🧽 Function – The 🫁 Dynamics
- w_high recruitability = 🫧 reopening + ↑ Pp ➩ Vena cava compression → Systemic &
renal congestion
- w_low recruitability = Minimal volume gain + 🫧 overdistension + 💥 Vascular
compression + ↑ 🫁 VR ➩ renal impairment.
6. More research is needed to:
- Fine-tune PEEP settings
- Maximize 🫁 benefits
- ↓ 🧽 and systemic harm
7. Think beyond the lungs when ventilating ARDS patients!
⏳ TIME MANAGEMENT.
01:04:43
Round: 5 00:29:71 FInal comments
Round: 4 50:21:89 ART all
Round: 3 06:06:42 ART abstract
Round: 2 07:24:68 ART selection
Round: 1 00:21:12 Last JC 8 min
Codified by AAACC
Glossary:
👶🏼 = infants = infancy, bW = birth weight, hALT = high altitude, LBW = Low Birth Weight, Preg = pregnant, SGA = Small for Gestational Age, sPTB = Spontaneous Preterm Birth
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2021, IJGO, UK ➖ srMA ➕ 2524, 59 IN ➕ -Nov 11, 2020 ➖ P I C O:
- P: hALT pregnant
- I: preg hALT
- C: preg non-hALT
- O: pOC = hALT impact on LBW, SGA, SPTB | sOC = magnitude LBW
3. EVIDENCE:
- hALT physiological changes ➩ pregnancy adaptations + hypobaric hypoxia
- 👶🏼 born at hALT = "lighter” (LBW)
- LBW ↔ short/long-term uOC
- https://www.floodmap.net
4. METHODS.
- 𝗜𝗡 ➠
- 𝗘𝗫 ➠
- RANDOM ➠
- INTERV ➠
6. RESULTS
7. RATIONALE
8. LIMITATIONS
Friday, April 04 , 2025 at 18h30 at BO - 23h30 at BE
AMA, AHO, BAH, HIBN, AAQC
⏳ TIME MANAGEMENT.
01:48:53
Round: 7 04:24:00 Finish
Round: 6 37:28:01 Results
Round: 5 14:58:50 Methods + Inclusion
Round: 4 09:53:45 Introduction
Round: 3 07:54:63 ART abstract
Round: 2 10:10:66 ART selection
Round: 1 24:04:51 Past JC
Friday, April 25 , 2025 at 18h30 at BO - 23h30 at BE
AHO, HIBN, AAQC
2025 CC - Limitations of SpO2 FiO2-ratio f_ class_ + monitoring of ARDS (Erlebach) [R].pdf
Codified by AMA
Glossary:
ARDS = acute respiratory distress syndrome, C = ICU cockpit, DBs = databases, M = MIMIC-IV, MV = mechanical ventilation, PF = PaO2/FiO2, RLS = resource limited settings, S = SICdb, SF = SpO2/FiO2.
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2025, CC, CH ➖ retro_obs_cohort ➕ >700 ➕ 3 DATABASES (MIMIC-IV = 2008-2022, SICdb = 2013-2021, ICU cockpit = since 2016 ) ➖ P I C O:
* P: ARDS
* 🅸: SpO2, FiO2, PaO2 ➩ SF
* 🅲: NA ➩ PF
* O: pOC = accuracy (correct/total classifications) | sOC = accuracy per severity +
trending ability to correlate w_FiO2
3. EVIDENCE:
- New global definition ➩ SpO2/FiO2 (additional ↓O2 criterion) for RLS
- PF used by major interventional trials
- Simplicity + practicality ➩ most widely used surrogate
- Disadvantage ➩ ABG needed ➕ availability in RLS ➕ complications (vascular injury, 🩸
oma, 🪲 , thrombosis, nerve injury)
4. METHODS.
- 𝗜𝗡 ➠
* M = USA, 65k - 1h resolution
* S = Austria - 27k, 1-per-min data
* C = Switzerland - 2,4k - >200Hz, continuous signals
* ARDS population
* C = manually selection w_Berlin definition.
* S + M = ICD codes (9 and 10)
* ↓O2: PF≤300 ➩ MV, NIV, CPAP ➕ PEEP ≥5 or HFNO flow≥30.
* IF multiple admission, only the 1st was IN
- 𝗘𝗫 ➠ ECMO
- INTERV ➠ 3 datapoints ➕ severity based on thresholds
- DATA MANAGEMENT ➠ Datapoints for each ABG measurement:
* M = with hourly data, values were matched within a 30-minute window.
* C = ABG timing was identified using gaps in arterial pressure waveforms. If no gap =
within 15 min ← the ABG timestamp, median values from 5 to 2 minutes prior (FiO₂ and
SpO₂)
* S, FiO₂ and SpO₂ were matched with some time delay allowance (details cut off).
- ANALYSIS
* Confusion matrices
* Density plots
* Limitations: SpO2 🆚 SaO2 ➩ bias + precision
5. RESULTS
* Misclassification ➩ 33% of datapoints ➩ 84% more severe ▶ Explanation: Imprecision of
SpO2 + equation to transform SF to PF
* High dependence SF on FiO2 settings ➩ Implications: major TTO + limited capability to
track severity (<20% events)
* Severity comparison = 69% ➖ individual datapoints = 67%
* Performance = BEST in more severe PF
* SF ↑ estimated = 28%
* SF ↓ estimated = 2.9%
* Accuracy = different ↔ DBs ➩ C = second 🆚 S = minute 🆚 M = hour
⏳ TIME MANAGEMENT.
01:53:25
Round: 9 01:09:86 Summary
Round: 8 47:47:74 Wrap-up
Round: 7 21:09:56 Tables & Figures
Round: 6 04:51:09 Wrap-up
Round: 5 02:47:08 INTRO
Round: 4 21:58:44 Wrap-up
Round: 3 05:04:28 ART intro + abstract
Round: 2 03:42:78 ART selection
Round: 1 04:55:03 Past JC
2025 NEJM - Liberal or Restrictive Transfusion Strategy in Aneurysmal SAH (English) [R].pdf
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
CFR = case fatality rate, DCI = delayed cerebral ischemia, E&D = early & delayed, EQ-5D-5L = EuroQol five-dimension, five-level, FIM = functional independence measure, M_ = mean, RC = red cell, VAS = visual analogue scale
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS ➩ SAHARA ➩ 2025, NEJM, 23_c ➖ RCT ➕ 742 pxs (→ 725) ➕ 12 m ➖
P I C O:
- P: adults w_ ‘acute_aneu_SAH + anemia’
- 🅸: liberal transfusion (≤10 g/dL)
- 🅲: restrictive transfusion (≤8 g/dL)
- O:
* pOC = u🧠OC12m (≥4 m_Rankin; 0-6)
* sOC = f_INDEPENDENCE12m (FIM; 18-126) ➕ QOL (EQ-5D-5L utility index; -10.1–
0.95 + VAS; 0-100)
3. EVIDENCE:
- SAH
* Condition ➩ Severe + life-threatening
* Cause ➩ early MM + loss of productive life years
* CFR ➩ 8-67%
* Affects ➩ young + mostly ♀
* Clinical course ➩ complicated by E&D 🧠 INSULTS
* Survivors ➩ <1/3 = full recovery ➖ [substantial] = dependent living.
- ↓Hb
* >50% of SAH ↔ worse_clin_OC
* ↓DO2 = ↑ E&D 🧠 insults ↪ aneurysm rupture (DCI) MAJOR contributors ➩ poor 🧠
recovery.
- RC Transfusion
* Limited + conflicting
* Based on small OBS studies
* GL ➩ vague ⓘ
* Threshold is unknown
4. RESULTS
- pOC
* 725pxs (98%)
* uOC = 122/364 (34%) 🅸 🆚 136/361 (38%) 🅲 (p=0.22)
- sOC
* FIM* = 83 🅸 🆚 80 🅲
* EQ-5D-5L* = 0.5 in both
* VAS* = 52 🅸 🆚 50 🅲
* AdvEve† = similar in both
Friday, April 18 , 2025 at 18h30 at BO - 23h30 at BE
AMA, AAQC
⏳ TIME MANAGEMENT.
01:24:11
Round: 6 10:40:74 Summary with AMA
Round: 5 16:05:19 Wrap-up
Round: 4 43:37:05 Wrap-up + ART intro
Round: 3 07:20:46 ART intro
Round: 2 01:48:24 ART selection
Round: 1 04:39:83 Past JC
Friday, May 9 , 2025 at 18h30 at BO - 23h30 at BE
AMA, EAM, AAQC
2025 CC - The ventilator of the future_ key principles and unmet needs (marini) [persp].pdf
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
🫁 = lungs, Di = diaphragm, LV = left ventricular, MV = mechanical ventilation, P-SILI = patient self-induced lung injury, RMP = respiratory muscle pump, RR = respiratory rate, TP = transpulmonary, VD = dead space.
1. iMV ➩ conditioned gas + adequate ventilation energy ➩ 🫁 expansion to prevent ATELECTASIS + consequences.
2. iMV allows monitoring:
* Airway pressures
* Flows
* Frequency
* Vt
3. NEW ADVANCES = Flow delivery patterns + sophisticated online processing
4. Applications in ‘PO ventilation + NM weakness’ ➩ machine incremental improvements
5. “Less than ideal for the most critically ill”
6. Technology + engineering ➩ ↗ capability + safety
7. LIMITATIONS
* P-SILI
* Sysinchony
* Muscle fatigue
* ↓ O2
* Di_DYS
8. Tracking the NET physiologic effect of CV system requires (caregivers): Independent detection + integration.
9. ❝ expertise and time to spend at the bedside
10. Reaction is OK, but intermittent adjustment + reaction to alarms = dangerous
11. Primary hazards:
* HD impairment
* VILI
* Impairment RMP
12. Insufficient surveillance + complex interactions among organs ➩ vary w_training + expertise of caregivers = universal PROBLEM.
13. GL not enough
* Helpful as 1st approximations
* Imprecise definition of: DIS OR synd + clinical trial.
* ∑ limit personalization.
14. ❝ no single set of parameters would suit all patients
15. UNMET GOALS of VENTILATORY support
* GAS EXCHANGE
* PAP ➩ disrupts homeostasis V/Q
* MV ↑ FiO2 + ↑ TPaw ➩ ∑ ✖ atelectasis ↗ O2, PROBLEMS:
* ↑ Pp ∑HD compromise + 💧 retention.
* Overdistention of aerated 🫁 zones ➩ suboptimal reperfusion ∑↑VD
* HDs
* ↑ intrapleural + → atrial pressure ➩ ↓ venous return + ↑ pre-capillary 🫁 vasculature
PRESSURE.
* ATRIAL pressure ➩ → ventricle ➩ LV filling ➩ ↓ CO… provokes ➩ Reflex fluid
loading (caregiver) ➩ ⊕ fluid balance (compressive forces on alveoli):
* Lung edema
* Pleural effusion
* Ascitis
* 🫁 injury
* VILI ➩ Tidal repetition excessive tissue strains produced by the energy of 🫁
distension.
* Extensively investigaged in LABS, less at bedside
* DIS type, stage and local environment = parenchymal VULNERABILITY (stress
threshold)
* HAZARDS = TP airspace pressure (analogue of tissue stress) + power (mechanical
energy * RR)
⏳ TIME MANAGEMENT.
01:53:25
Round: 9 01:09:86 Summary
Round: 8 47:47:74 Wrap-up
Round: 7 21:09:56 Tables & Figures
Round: 6 04:51:09 Wrap-up
Round: 5 02:47:08 INTRO
Round: 4 21:58:44 Wrap-up
Round: 3 05:04:28 ART intro + abstract
Round: 2 03:42:78 ART selection
Round: 1 04:55:03 Past JC
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2021, IJGO, UK ➖ srMA ➕ 2524, 59 IN ➕ -Nov 11, 2020 ➖ P I C O:
P: hALT pregnant
🅸: preg hALT
🅲: preg non-hALT
O: pOC = hALT impact on LBW, SGA, SPTB | sOC = magnitude LBW
3. EVIDENCE:
- …
4. METHODS.
- 𝗜𝗡 ➠
- 𝗘𝗫 ➠
- RANDOM ➠
- INTERV ➠
5. RESULTS
6. RATIONALE
7. LIMITATIONS
Friday, May 2 , 2025 at 18h30 at BO - 23h30 at BE
BLAS, HIBN, AAQC
⏳ TIME MANAGEMENT.
01:19:21
Round: 3 59:56:38 The rest
Round: 2 01:59:03 ART selection
Round: 1 17:26:31 Past JC
Friday, May 23 , 2025 at 18h30 at BO - 23h30 at BE
AMA, AHO, BAH, GMC, HIBN, AAQC
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (MAAT)
Glossary:
Com = complement, coa_factors = coagulation factors, DAMPs = damage-associated molecular patterns, M = monocytes, N = neutrophils, OD = organ dysfunction, PLT = platelets, PRRs = pattern recognition receptors, ROS = reactive oxygen species.
1. Sepsis definition
2. 11M deaths per year ➕ 49M cases
3. Advancements ➩ S• immunobiology = ↗️ nuanced conceptualization (resistance, tolerance,
resilience, resolution, repair)
4. Immunothrombosis ➩ immune ➕ coagulation ➩ to ✖ pathogens
* ⊕ cellular + molecular ➩ N, PLT, M, com, DAMPs, coa_factors
* ⊕ excesive + uncontrolled ➩ thromboinflammation
5. DAMPs ➩ danger signals ▶ triggers INFLAMMATORY RESPONSES thought PRRs:
* TLR
* NOD
6. ↑ DAMPs ➩ amplifies + perpetuates 📈INFLAMMATION ➩ S• + OD
7. NETs ➩ histones + granular proteins ➩ TRAPS
8. ↑ FORMATION ± DYSREGULATED clearance ➩ pathophysiology of S• + thrombosis
9. N ➩ short lifespan = 5-7d ➩ ↓ once ACTIVATED:
- (+) rapid response to INF
- (-) obstacle to research (isolate cells + expand ➩ in vitro)
- Few hours life AFTER ISOLATION
- Triggers: PROCESSES ➩ degranulation + ROS
10. N requires PLT + M to get activated (makes it harder to study in vitro)
11. N have different PHENOTYPES + PROFILES (functionals) ➩ still being explored.
12. Not only affect BLOODSTREAM, but also TISSUES
13. Sophisticated techniques are needed (not universally available). E.g. intravital microscopy
14. Ethical and technical CONSIDERATIONS make it difficult to study in humans.
15. 2004. Brinkmann ➩ nuclear content ➩ traps + kill bacteria ➩ scepticism (short-lived
concept challenged)
16. 2007. Fuchs ➩ net formation was triggered by NETosis (active cell detah) ➩ requires ROS
by NADPH.
17. NEt release ⊕ stimuli:
- Bacteria
- Viruses
- Fungi
- Parasites
- Pro-inflammatory mediators: IL8, lymphotoxin-alpha
Friday, May 16 , 2025 at 18h30 at BO - 23h30 at BE
AMA, HIBN, AAQC
2025 JAMA - Metformin for Knee Osteoarthritis in Pxs W_ Overweight or Obesity (pan) [RCT].pdf
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
ACR = American College of Rheumatology, AMPK = Adenosine Monophosphate–Activated Protein Kinase, ES = Effect Size, 💉 = Intravenous, OA = Osteoarthritis, VAS = Visual Analog Scale..
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2025, JAMA, AUS ➖ par_db_RCT ➕ 54 🆚 53 ➕6m of intervention – total 2y (2021 to 2023), last f-up Feb 2024 ➖ P I C O:
- P: symp_knee OSTEOARTHRITIS + overweight OR obesity
- 🅸: metformin 2g/d
- 🅲: placebo
- O: pOC = change in knee pain (VAS) | sOC = WOMACS + AQoL
3. EVIDENCE:
- Preclinical + preliminary ➩ ↓ inflammation ➕ preserves cartilage ➕ ↗ knee pain
- OA IN 365M
- Knee OA ➩ ↑ weight joints, inflammation, imp_GLU & LIP metabolism ▶ SYST
inflammation + oxidative stress + metabolic DYS in JOINT TISSUES (cartilage degradation
+ DIS progression)
- METFORMIN >60y known as 1st line for DM
- SAFE, inexpensive, well-tolerated biguanide
- ↓ liver_GLU production ➕ ↓ IR ➕ ↓ ENDOGENOUS hyperINSULINEMIA
- Modest weight loss ➕ ↓ inflammation (w_ & wo_DM)
- PLEIOTROPIC EFFECTS: ↓ knee pain in OA
* Inflammatory properties
* ↑ GLU & LIP metabolism ➩ ↑ ⊕ AMPk
4. METHODS.
- 𝗜𝗡 ➠ pain (>4/10 VAS) ➕ BMI ≥25 ➕ >40yo ➕ ≥6m pain➕ know OA by criteria ACR
- 𝗘𝗫 ➠ sev_Xray knee OA (Kellgren-Lawrence grade 4) ➕ Severe knee pain (>80 mm
VAS) ➕ Inflammatory arthritis ➕ Significant knee injury ➕ DM ➕ Knee surgery (past
year or next 6 m) ➕ Intra-articular hyaluronic acid 💉 (past 6 m) ➕ Corticosteroid 💉
(past 3 m) ➕ investigational drug or device (30d prior to randomization) ➕ Conditions
affecting lower limb function (NEURO disorders, stroke) ➕ ♾ & liver IMPAIRMENT.
- RANDOM ➠ contacted by website, email, phone ➕local and social media
advertisements.
- Physical examination not performed by a physician ➩ participants reported KNEE
CREPITUS + TENDERNESS + WARMT + bony enlargement ✖
- INDEX KNEE:
* The symptomatic OA knee
* IF both SYMP + eligible VAS ➩ ↑VAS ✔
* If pain levels = ➩ less severe Xray ✔
* IF both identical ➩ dominant ✔
- INTERV ➠ Telemedicine (remote follow-up)
- DESIGNS: Originally 2 studies ➕ 2 ethical committees ➕ funding only for study 1
➕CONSORT
5. RESULTS
- pOC:
* 🅸 ↓ 31.3 mm 🅲 ↓ 18.9 mm
* ES: 0.43 (95% CI: 0.02 to 0.83); P = .01
- sOC – WOMAC Scores:
* Pain Subscale ➩ 🅸 : ↓ 113.9 🅲 : ↓ 68.2 ➖ Adjusted DIFF: –42.4 (95% CI: –83.9 to –
1.0); P = .045
* Stiffness Subscale ➩ 🅸 : ↓ 56.9 🅲 : ↓ 26.7 ➖ Adjusted DIFF: –23.0 (95% CI: –40.4 to –
5.7); P = .01
* Function Subscale ➩ 🅸 : ↓ 426.1 🅲 : ↓ 221.7 ➖ Adjusted DIFF: –179.8 (95% CI: –313.0
to –46.6); P = .009
- oOC
* AQoL-8D ➩ 0.01 (95% CI: –0.02 to 0.05); P = .47
* OMERACT-OARSI Responder ➩ 🅸 : 65% responders 🅲 : 45% responders ➩ OR: 2.21
(95% CI: 0.92 to 5.31); P = .07
* VAS Change 3m ➩ DIFF: –2.5 mm (95% CI: –11.7 to 6.6 mm); P = .58
⏳ TIME MANAGEMENT.
01:44:07
Round: 6 00:22:58 Comment
Round: 5 54:52:26 Wrap-up + analysis
Round: 4 30:43:87 Abstract + intro
Round: 3 06:51:44 ART selection
Round: 2 09:40:43 Past JC
Friday, June 20 , 2025 at 18h30 at BO - 23h30 at BE
AMA, HIBN, AAQC
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
🫃🏽 = abdomen = abdominal
1. ♀ 30yo ➩ SYMP = fever + 🫃🏽pain
2. H+ 6d af_DELIVERY | 35w + colonization B streptococcus (vancomycin) + spontaneous rupture membranes + 8h later: infant of 3,5Kg, large for gestational age.
3. 4d af_DELIVERY ➩ mild diffuse 🫃🏽 & PELVIC cramping + vaginal bleeding (clots).
4. Admission ➩ fever + chills
- Inguinal area w_bumps (small + painful), drained blood & pus
- Leg swelling (abated since childbirth)
5. CLINICS ➩
- T 38,7 ➕ BP 125/80
- Erythematous pustules drained yellow, purulent fluid (right inguinal area)
- Scarring (left inguinal area)
- LEU 22,9
- Blood and cervical cultures
6. HISTORY
- Epiploic appendagitis 10w before ADM
- Acetaminophen + ibuprofen for 🫃🏽 pain
- Amoxicillin + cephalexin = caused HIVES
- Father and paternal grandfather ➩ arthritis
- Brother ➩ Crohn’s disease
- Brother ➩ neurofibromatosis
7. CT Abdomen & pelvis
- Normal
- Mild adjacent fat
8. INFECTO
- Genta + clinda
- Endometritis
- Fever + 🫃🏽 pain + ↑ LEU
- Vanco on D3
- Cefepime on D4 (once = TEST DOSE) ➩ ✔ ➩ genta + clinda ✖
- Vanco + cefepime + metro
9. PATHOLOGY
- D6, biopsy ➩ neutrophilic debris (dense neutrophilic infiltrate)
10. MRI
- Angio MRI ➩ ascitis + anasarca
- 4D later ➩ ↑ ascitis + anasarca ➩ 2 new fluid collections
* Left parametrical 6.3
* Right uterocervical junction 3.2
11. INFECTO
- Cefepime + metro ✖
- Vanco ✔ + MERO (due to fever)
- Catheter into left parametrial fluid collection (20mL purulent fluid) drained ➩ cultures no
growth
12. CLINICS
- D11. SpO2 86% AA ➕ O2 2L ➩ ↗️ SpO2 91%
- T 36,7, BP 109/58, HR 112 (regular), RR 24
- Tired and ill
- Marked jugular venous distention
- Scant purulent drainage (percutaneous catheter)
- Anasarca ➕ symmetric 1+ ankle edema
13. LABS
- Inflammation clearly shown
- Biventricular ok, right atrium and right ventricle DILATED + septum flattened d_dyas -
pulmonary arteries DILATED
14. IMAGENO
- No PE, yes sub segmental atelectasis
- ↑ ascitis and anasarca
- Splenomegaly + hepatomegaly
- Collection resolved
- Right remained unchanged
- Liver enzymes ABNORMAL ➩ cholangiopancreatography = multiple intrahepatic fluid
collections = hyperintensty T2-wighted
15. D12.
- Plaques ➩ in the peripheral IV catheter
- Bulla ➩ left abdominal wall
- Plaques ➩ ulcerated
- New skin lesions ➩ Right inguinal crease and mons pubis
16. Next 2 days
- Bulla ➩ ulcerated
- Another lesion in percutaneous drainage catheter
- ↑ area & depth ➩ left upper arm, right inguinal crease, mons pubis
- Furosemide
- Vanco ✖ , mero ✔ , DAPTOMICIN + MICAFUNGIN started
17. DIFFERENTIAL
- Hepatobiliar source ➩ ↑ ALK Phosp ➕ GGT
- Biopsy does not allow us to exclude ENDOMETRITIS
- Fungal + mycobacterial INF should be considered ➩ empirical ATB without results +
new collections + ↑ HR + ↑ RR + ↑ hypoxemia + negative cultures
Friday, June 13 , 2025 at 18h30 at BO - 23h30 at BE
AMA, MAAT, AAQC
2025 EHJ - Heart rate-lowering drugs+outcomes in HTA+CVD a MA (Sanidas) [RCT].pdf
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
CHD = Coronary heart disease, MACE = Major CV events, MI = myocardial infarction, S† = Stroke.
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2025, EHJ, GR ➖ srMA ➕ 74 RCT (>150k pxs) ➕ - July 2024 ➖ P I C O:
- P: HTA ± CVD
- 🅸: HR↓ over 2,7y
- 🅲: PLACEBO + less intense TTO
- O:
1. CHD (Coronary † ➕ Non-fatal MI
2. S† (Fatal ➕ Non-fatal)
3. Hº-HF (Hº d_ HF)
4. MACE (Composite: S† + CHD)
5. Expanded composite CV events (Composite: S† ➕ CHD ➕ HF or MACE)
6. CV†
7. acMM
8. AdvEve w_ TTO ✋🏽 (Serious AdvEve → permanent TTO ✋🏽)
3. EVIDENCE:
- …
4. METHODS.
- 𝗜𝗡 ➠
• RCTs w_ parallel design
• On-TTO ƒ-up ≥6m
• HR Δ between arms: ≥2 b.p.m.
• Trials where:
• HR↓ 🆚 non-HR-lowering agents
• More- 🆚 less- intense HR-lowering agents
• Non-intended HR Δ ≥2 b.p.m. occurred
• HR↓ randomized on background of other HR↓ therapies or added per protocol
• Any comorbidities, incl. AF or CKD (incl. dialysis)
- 𝗘𝗫 ➠
• HR Δ <2 b.p.m. between arms
• Cross-over designs
• Sub-studies of main trials
• Trials wo_ HR data d_ ƒ-up
• Trials <6 mo ƒ-up
• Trials w_ <5 total events
⏳ TIME MANAGEMENT.
01:49:03
Round: 6 15:51:49 Comment
Round: 5 51:28:43 Method
Round: 4 19:10:37 intro
Round: 3 12:18:10 ART abstract
Round: 2 04:23:64 ART selection
Round: 1 05:51:08 Last JC
Friday, July 18 , 2025 at 18h30 at BO - 23h30 at BE
MASP, AAQC
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
† = deaths, HC = hydrocortisone, ID = identification, MEDs = medications, ML = machine learning, PLA = placebo, VP = vasopressin
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2025, ICM, UK ➖ 2_db_RT ➕ LeoPARDS (<1,5k samples, >400pxs) & VANISH (<500 samples, >170 pxs) ➕ LeoPARDS (Jan 2014 - Dec 2015) & VANISH (Feb 2013 - May 2015) ➖ P I C O:
- P: SØ metabolic clusters
- 🅸: serum at 4 time points – LeoPARDS = derivation ➕ VANISH = validation.
- 🅲: NA
- O: pOC = MM | sOC = cluster membership ↔ 28d_OC ➕ SOFA mean tatal ➕ interaction
“trial TTO ↔ baseline cluster membership” on OC
3. EVIDENCE.
- S• ➩ 11M † per year ➕ 20% of global †
- TTO limited ➩ failure is due to HETEROGENEITY
- ML was applied to make progress on TECHNIQUES to biological data:
* Gene expression
* Inflammatory proteins.
- Questions are:
* Are sub-phenotypes stable?
* Is transition ↔ sub-phenotypes are predictable of OC?
- Metabolomics ➩ measurement of small molecules → host ↔ environment (encapsulate
wide range of origins: genome, proteome, pathogen)
- Many studies exposed DX, prognosis and pathogen ID in S•
- Few studies used metabolois to ID S• sub-phenotypes (DEF: not apparent to clinicians +
note yet validated)
- MEDs used in S• (vasopressin, levosimendan, glucocorticoids) could show heterogeneity of
TTO based on px METABOLIC profiles.
4. METHODS.
- 𝗜𝗡 ➠ S• + 6h vasopressor ➩ randomized to VP or NE, followed by HC or PLA (last 2 given
ONLY if max infusion of the 1st study drug was reached)
- RANDOM ➠ Hierarchical, k-means, consensus clustering ➩ applied to ID “metabolic sub-
phenotypes”:
* 70% derivation (LeoPARD)
* 30% validation (VANISH)
5. RESULTS.
⏳ TIME MANAGEMENT.
01:49:26
Round: 4 03:39:44 Comments
Round: 3 01:31:22 ART
Round: 2 08:02:32 ART selection
Round: 1 06:22:58 Past JC
- The 3 metabolic subgroups EVOLVE over time
- Low lysophospholipid sub-phenotypes ↔ ↑ MM
- Monitoring could help ID:
* pxs at r_poor_OC
* Direct novel therapies (lysophospholipid supplementation)
Friday, August 15 , 2025 at 18h30 at BO - 23h30 at BE
AMA, MASP, HIBN, AAQC
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
ACIP = CDC Advisory Committee for Immunization Practices, ANH = acute normovolemic hemodilution, ARC = allogenic red-cell tranfusion, COR = class of recommendation, CPB = cardiopulmonary bypass, IO = intraoperative, LOE = level of evidence, NA = North America, TACO = transfusion-associated circulatory overload, TRALI = transfusion-related lung injury, UC = usual care, 🦠 = infections, 🤧 = allergic reactions, 🥶 = chills, 🌡️ = fever.
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS ➩ 2025, NEJM, IT ➖ mn_sb_prag_RCT ➕ 32 centers, 11 countries (NA, SA, EU, ASIA) ➕ … ➖ P I C O:
- P: 🫀 Sx w_CPB
- 🅸: ANH
- 🅲: usual care (ARC)
- O: pOC = transfusion of ≥1 unit of ARC | sOC = ac_MM30 af_Sx OR d_H+ ➕ bleeding
complications ➕ ischemic ➕ AKI.
3. EVIDENCE.
a. 10M of RCU transfused (USA) per year
b. 3 main concerns: costs ➕ shortages ➕ transfusion-related complications
c. COST ➩ $150 - $634 per unit (country dependent).
d. AVAILABILITY ➩ fluctuates over time w_periods of shortages ▶︎ postponement of
nonurgent Sx
e. DELAYS ➩ affect: px health ➕ costs
f. RISKS ➩ mild🌡️, 🥶, 🤧, 🦠, TRALI, TACO (1-5%)
g. 🫀 Sx anually (worldwide) ▶︎ >2M pxs ➖ 35% receive ≥1 URC
h. ANH ▶︎ 20% 🫀 Sx (USA) ➕ 27% 🫀 anesthesiologists ➕ 14% pxs wordwide. (before
heparin + CPB)
i. RETROSPECTIVE ➩ 18k pxs, USA, 🫀Sx ➩ OCs:
i. ANH only (LOWEST % of IO transfusion)
ii. retrograde autologous priming only
iii. both
iv. neither
j. MA ➩ 29 RCT, 🫀Sx, USA + 10 others ➩ ↓ need of URC w_ANH ▶︎ $magnified$ when
≥650mL was withdrawn preOP.
k. MA ➩ RCTs ▶︎ ANH = ↓ % pxs ➕ ↓ number URC.
l. GL 2021 ACP * ANH is a reasonable method to reduce bleeding and transfusion
m. GL 2024 EU ** ANH may be considered to reduce postoperative transfusions
(LOE A, COR IIb)
n. Consensus statement ▶︎ studies were underpowered to assess SAFETY + HD
procedures varied among studies.
4. METHODS.
- 𝗜𝗡 ➠ low-dose aspirin was permitted.
- 𝗘𝗫 ➠ unstable CAD ➕ critical periOP state ➕ ER Sx ➕ inadequate DC antiCOAG or
antiPLAT. 2nd screening ➩ r_HD instability OR anemia af_ANH.
- RANDOM ➠ Web-based system, computer generated, permuted-block sequences,
w_stratification (sites).
- INTERV ➠ ≥650mL of whole blood w_crystalloid replacement if needed.
- 3mL of crystalloids / 1mL withdrawal, stored, reinfused.
- heparin reversed w_protamine
- Withdrawn w_large-bore, central, rapid-infusion catheter
- Thresholds: <28% ← CPB, <20% d_CPB, <25% immediately af_CPB weaning, <27%
d_PO H+ stay.
- If anemic ← or d_ANH = transfusion (anesthesiologist)
- BLINDED ▶︎ pxs, investigators, data collectors, OC assessors, statisticians.
5. RESULTS.
- 2010 randomized ➩ 1010 ANH 🆚 1000 UC
- One ARC ▶︎ 27% ANH 🆚 29% UC (p=0.34)
- Bleeding ▶︎ 4% ANH 🆚 3% UC
- MM30 ▶︎ 1,4% ANH 🆚 1,6% UC
- Safety ▶︎ were SIMILAR in both
⏳ TIME MANAGEMENT.
02:19:33
Round: 5 00:58:20 Close
Round: 4 01:14:45 Wrap-up
Round: 3 53:46:91 Reading + notes
Round: 2 04:03:97 ART selection
Round: 1 05:58:64 Past JC
Friday, August 8 , 2025 at 18h30 at BO - 23h30 at BE
AMA, AHO, RAH, HIBN, YZE, AAQC
2025 JAMA - The CDC No Longer Recommends C19 Shots During Pregnancy Now What (rubin) [mn].pdf
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
ACIP = CDC Advisory Committee for Immunization Practices, VAX = vaccines, VRBPAC = FDA’s Vaccines and Related Biological Products Advisory Committee.
1. Kennedy ▶︎ announced he had removed C19 vax for: healthy children + pregnant ♀
(video in X)
2. Kennedy = founder and former chair of antivaccine organization Children’s Health Defense.
3. NIH + FDA had repesentatives, BUT no one from the CDC.
4. No one explain why the annoucement. (the rationale)
5. Confusing ➩ people involved publisehd a week earlier ➩ NEJM = CDC list of undelying
ondicions that ↑r_sC19: pregnancy + recent pregnancy.
6. 4 weeks after the announcement ➩ ACIP (created in 1964) 1st meeting EMPHASIZED ▶︎
IMP C19 vax d_pregnancy.
7. MacNeil (CDC respiratory viruses Branch) ▶︎ vax protect pregnant ♀ + infants + severe DIS
8. 17 panelists from ACIP were fired before the announcement. The new ones did not note the
CONTRADICTION with the epimedio data.
9. Medical profesional independent groups started to develop + promote their OWN ★
10. VRBPAC ▶︎ May 22 = continue C19 VAX during fall ➕ TARGET JN.1 (or on of its
descendants). Asked to manufacture monovalent + JN.1-lineage based VAX.
11. Brewer ▶︎ one of the 17 fired ACIP panelists ➩ ❝we need to vaccinate pregnant women to
protect those kids and protect the pregnancy itself.
12. ACIP agenda ➩ 3 regular meeting yearly: August, September, October.
13. Panagiotakopoulos ▶︎ decided to quit, worked for 12 years… did not agree with the
announcement.
14. Access ➕ insurance are AFFECTED. (pharmacist won’t vaccinate even if you want it)
15. Riley (laison: ACOG ↔ ACIP) ▶︎ reviewed new vax’s safety METICULOUSLY with her team
➩ makes her angry “…. biased in our deliberations”.
16. Muñoz (laison: IDSA ↔ ACIP) ▶︎ did not attend, either online.
17. Anyhow, new ACIP voted:
a. clesrovimab ➩ newly approved anti-RSV mAb ➩ <8m (mothers not vax)
b. flu vax without thimerosal ➩ ≥6m
c. thimerosal-free flu vax ➩ ♀ + children + adolescents through 18yo.
18. Many antiVAX groups are taking advantage of the situation. 19. Gorham ▶︎ ❝ lives are at
risk, and decades of public health and trust are being actively and carelessly undermined.”
⏳ TIME MANAGEMENT.
02:29:16
Round: 10 02:13:20 Comments
Round: 9 29:43:66 Wrap-up
Round: 8 22:37:99 Analysis
Round: 7 28:44:28 Reading + notes
Round: 6 06:07:19 Reading + notes
Round: 5 30:40:10 Analysis
Round: 4 06:44:94 Reading + notes
Round: 3 07:54:37 ART selection
Round: 2 00:20:40 Comments
Round: 1 14:10:54 Past JC
Friday, August 29 , 2025 at 18h30 at BO - 23h30 at BE
JJFM, MASP, AAQC
⏳ TIME MANAGEMENT.
02:29:16
Round: 10 02:13:20 Comments
Round: 9 29:43:66 Wrap-up
Round: 8 22:37:99 Analysis
Round: 7 28:44:28 Reading + notes
Round: 6 06:07:19 Reading + notes
Round: 5 30:40:10 Analysis
Round: 4 06:44:94 Reading + notes
Round: 3 07:54:37 ART selection
Round: 2 00:20:40 Comments
Round: 1 14:10:54 Past JC
2025 JAMA - Higher Educational Attainment and Accelerated Tau Accumulation in Alzheimer Disease (cai) [R].pdf
Codified by 𝙄𝙉𝘼𝘼𝙌𝘾 ᴮᴼ (ABFL)
Glossary:
🧠 = brain
🫁 = lungs
🫀 = heart
🫃🏽 = abdomen = abdominal
♾️ = kidneys = renal
🩸= blood = hematology
🪲 = infections
💨 = flow
➰ = pressure
🤓 = analysis;
⚡️ = cardiac arrest;
📈 = arrhythmia;
🗣 = suggestion(s)
★ = recommendation(s)
AD = Alzheimer disease;
TTO = treatment
Aß = amiloid beta (ß)
h_EA = high educational attainment
1. 𝙄𝙌𝘾 BS ➩ Y, J, C ➖ T ➕ N ➕ t ➖ P I C O:
2. 𝙄𝙌𝘾 BS 🟰 2025, JAMA, CH ➖ analysis_3cohort ➕ 887 = >350 (ADNI), <400 (A4),
>100 (GHABS) ➕ -Nov 11, 2020 ➖ P I C O:
- P: adults
- Aß⊕ & Aß⊖
- ADNI 73yo | A4 72yo | GHABS 66yo
- 🅸: h_EA
- 🅲: l_EA
- O:pOC = tau changes | sOC =
1. interactions w_aßburden ➕ entorhinal tau ➕ p-tau217 (Aß⊕)
2. Connectivity-associated tau spread (Aß/EA groups)
3. Treatment attenuated tau accumulation (Aß⊕ h_EA)
3. EVIDENCE.
a. Aß plaques + neurofibrillary tau tangles:
i. AD hallmarks.
ii. PET detected
b.Lista
4. METHODS.
- 𝗜𝗡 ➠
- 𝗘𝗫 ➠
- RANDOM ➠
- INTERV ➠
5. RESULTS.
a. Aß⊖ ➩ `tau accumulation:`h_EA < l_EA (*p=.03*)
b. Aß⊕:
i. `Tau accumulation:` h_EA > l_EA (*p=.03*)
1. Aß-associated (*p=.006*)
2. Tau-associated (*p=.01*)
3. p-tau217-associated (*p=.04*)
4. connectivity-associated (p=.048)
c. Aß-targeting TTO ➩ mitigated p-tau217-associated (AD+h_EA) (*p<.001*)
d. ∑ ➩ h_EA ↔ faster `tau accumulation` ➕ `spread in Aß ⊕`
6. RATIONALE.
a. In AD & h_EA ➩ Aß clearance is IMP to ↓ `tau progression`
7. LIMITATIONS.